Pediatric cancer relapse prediction is becoming a pivotal focus in modern oncology, particularly with advancements in artificial intelligence (AI) technology. A groundbreaking study has demonstrated that AI tools can significantly enhance the prediction of relapse risk in children diagnosed with brain tumors, specifically gliomas. This approach surpasses traditional methodologies, offering more accurate assessments and potentially revolutionizing treatment protocols. By leveraging machine learning cancer prediction models to analyze consecutive brain scans, healthcare providers can identify which pediatric patients are at heightened risk of brain tumor relapse. As the landscape of children cancer treatment evolves, embracing these innovative predictive tools can lead to improved care and outcomes for young patients.
Predicting the recurrence of childhood cancers, especially brain tumors, has traditionally posed a significant challenge for oncologists. Innovations in technology, particularly in AI applications within pediatric oncology, are paving the way for advanced methods of evaluating glioma recurrence risk. Utilizing machine learning techniques, healthcare practitioners can now monitor patients’ health more effectively and anticipate potential relapses. This shift not only alleviates the stress associated with frequent imaging but also tailors treatment strategies to individual needs. By enhancing our understanding of relapse patterns, we can better support young patients and their families in navigating the complexities of cancer care.
The Role of AI in Pediatric Oncology
In recent years, the integration of artificial intelligence (AI) into pediatric oncology has revolutionized the way we approach cancer treatment and prediction. AI tools have emerged as powerful adjuncts in identifying patterns that are often missed by human analysis alone. By employing machine learning algorithms, researchers can analyze vast amounts of data, including imaging studies and clinical histories, to enhance the accuracy of cancer predictions. This shift towards automated analysis not only improves diagnostic precision but also paves the way for personalized treatment strategies that adapt to the unique needs of each pediatric patient.
One of the most significant advancements in this field is the use of AI in predicting glioma recurrence risk in children. Traditional methods centered on single images often fall short, misrepresenting the true risk of relapse. With AI’s ability to synthesize data from multiple imaging time points, practitioners can gain a clearer picture of a patient’s prognosis. As a result, families can make more informed decisions regarding treatment plans and follow-up care, reducing anxiety associated with frequent medical evaluations.
Understanding Glioma Recurrence Risk
Gliomas are a type of brain tumor that can affect children, with treatment outcomes varying significantly based on the tumor’s grade and location. The challenge lies in accurately predicting which patients are at a higher risk of glioma recurrence after initial treatment. Recent studies have demonstrated that the use of AI-driven temporal learning can identify subtle changes in brain scans over time that indicate an increased likelihood of relapse. This groundbreaking approach not only improves prediction accuracy but also allows for more targeted intervention strategies.
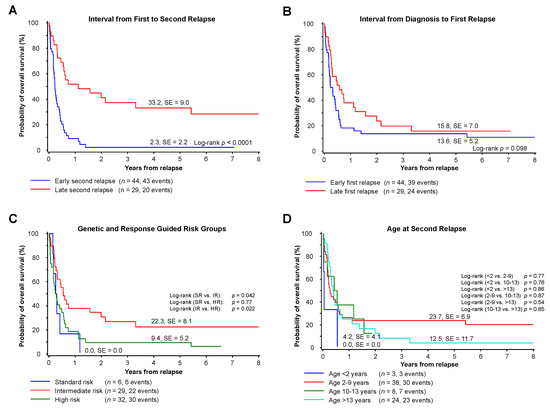
With AI tools showing predictive accuracies ranging from 75-89% compared to traditional methods that offer predictions as low as 50%, the potential impact on patient care is profound. By understanding glioma recurrence risk more clearly, healthcare providers can minimize the frequency of imaging for low-risk patients, thereby alleviating the burden of unnecessary stress on children and their families. Conversely, high-risk patients can receive preemptive treatments designed to tackle potential relapses, enhancing overall treatment outcomes.
Machine Learning and Cancer Prediction in Children
Machine learning has become an invaluable resource in pediatric cancer prediction, utilizing sophisticated algorithms to identify patterns and risks that may not be evident to medical professionals. This technology is particularly effective in managing brain tumors, where continuous monitoring is essential due to the unpredictability of disease progression. By analyzing historical data from pediatric patients, machine learning models can be trained to forecast the likelihood of cancer relapse, enabling clinicians to develop tailored treatment plans that address individual patient needs.
Incorporating machine learning into the care continuum allows for better management of resources and improved outcomes in children undergoing cancer treatment. Predictive analytics can guide decisions regarding the frequency of medical imaging and interventions, effectively streamlining patient care. Furthermore, as more data is gathered and models refined, the potential for machine learning to transform pediatric oncology continues to grow, leading to more precise and hopefully successful treatment outcomes.
The Impact of Brain Tumor Relapse
The emotional and physical toll of brain tumor relapse on pediatric patients and their families can be profound. When a child faces a recurrence, it not only complicates the treatment journey but can also lead to increased anxiety and fear among patients and their caregivers. Relapses can result in more intensive treatments, longer hospital stays, and the need for multiple therapeutic approaches, thus emphasizing the importance of early identification of recurrence risk.
Understanding the impact of brain tumor relapse highlights the necessity for innovative tools that can predict such outcomes. With advancements in AI and machine learning, healthcare providers can offer better management of care, aiming to improve survival rates and quality of life for young patients. By harnessing the capabilities of these technologies, we move closer to a future where advanced predictive tools minimize the risk and repercussions of relapses in patients suffering from pediatric brain tumors.
Advancements in Children Cancer Treatment
The burgeoning field of AI in pediatric oncology is ushering in a new era of advancements in cancer treatment for children. Traditional cancer treatments, often based on age-old protocols and trial-and-error approaches, are evolving as new technologies allow for more personalized and effective care plans. Tailored treatments based on predictive analytics from AI tools ensure that each child’s unique biology and tumor characteristics are considered in their care.
By leveraging current developments in AI and machine learning, oncologists can design treatments that are not just reactive but proactive. This shifts the paradigm from traditional treatment methods to one that focuses on preventing recurrences before they occur, which is particularly critical for pediatric patients. Early intervention strategies, informed by AI’s predictive capabilities, could significantly improve long-term outcomes for children battling cancer.
The Future of AI in Pediatric Oncology
As research continues into the capabilities of AI within pediatric oncology, the future looks promising for both patients and healthcare providers. Ongoing studies aim to refine the predictive models used to evaluate cancer risk, particularly focusing on the intricacies of various tumor types, including gliomas. The aspiration is to develop robust AI applications that are seamlessly integrated into clinical practice, enhancing both the accuracy and efficiency of patient assessments.
One of the most exciting prospects is the potential for AI to facilitate real-time monitoring of pediatric patients. By combining AI tools with telemedicine, healthcare providers could continuously analyze patient data and adjust treatment protocols dynamically, ensuring that the highest standards of care are maintained. Enhancing surveillance and intervention strategies could significantly ease the burden on families and improve the quality of life for children undergoing cancer treatment.
Clinical Trials and AI-Driven Predictions
The success of AI in predicting pediatric cancer relapse hinges on rigorous clinical validation. As research teams, including those from esteemed institutions, move forward with their findings, the next crucial step is to implement clinical trials that test the efficacy of these AI-driven predictions in real-world settings. Such studies will be instrumental in determining how these advanced technologies can be included in routine clinical practice to optimize outcomes for young patients.
Through the establishment of clinical trials, researchers aim to explore how AI’s predictive capabilities can be used not only to advise on imaging frequency but also on therapeutic strategies for young patients at risk of recurrence. By evaluating the impact of these tools on patient care, they hope to solidify the role of AI in influencing treatment trajectories, ultimately leading to more precise and effective treatment plans in pediatric oncology.
Reducing Imaging Frequency for Low-Risk Patients
One of the significant implications of enhanced AI predictions in pediatric oncology is the potential for reducing the frequency of imaging in low-risk patients. Children undergoing treatment for brain tumors often face stringent follow-up protocols that can be both psychologically taxing and physically demanding. By employing AI tools to accurately identify which patients have a lower probability of recurrence, medical teams can adjust follow-up schedules accordingly, minimizing the need for unnecessary MRI scans.
This not only alleviates the stress associated with frequent imaging procedures but also allows healthcare resources to be utilized more effectively. With fewer imaging appointments, families can experience reduced logistical burdens while focusing their attention on supportive care and recovery. Ultimately, the goal is to ensure that those who need close monitoring receive it, while also freeing up resources for other critical areas of pediatric cancer care.
The Importance of Early Risk Identification
Early identification of relapse risk in pediatric cancer patients is paramount for effective treatment and management. With advances in AI, the potential to pinpoint high-risk patients early in their care journey could lead to the implementation of targeted therapeutic interventions that directly address the likelihood of recurrence. This proactive approach can ensure timely access to the necessary treatments that can significantly alter patient outcomes.
Furthermore, understanding patients’ risk profiles early on can lead to informed discussions between healthcare providers and families regarding treatment options. This openness fosters an environment of trust and collaboration, where families can engage actively in their child’s treatment journey. The emphasis on early identification not only promotes better health outcomes but also enhances the overall experience for families faced with the challenges of pediatric cancer care.
Frequently Asked Questions
How does AI predict pediatric cancer relapse risk in children with gliomas?
AI predicts pediatric cancer relapse risk by analyzing multiple brain scans over time, utilizing a method known as temporal learning. This technology synthesizes information from serial imaging, allowing it to identify subtle changes that might indicate a risk of brain tumor relapse more accurately than traditional single-image approaches.
What is the significance of machine learning in pediatric cancer relapse prediction?
Machine learning plays a vital role in pediatric cancer relapse prediction by improving the accuracy of risk assessments. Algorithms trained on extensive datasets of brain scans enable healthcare providers to identify which children might be at higher risk for glioma recurrence, ultimately leading to more personalized and proactive treatment plans.
What are the advantages of using AI tools in pediatric oncology for predicting brain tumor relapse?
The advantages of using AI tools in pediatric oncology include enhanced prediction accuracy, reduced need for frequent imaging, and the ability to tailor treatment plans based on an individual child’s relapse risk. These benefits can significantly alleviate the stress and burden on children and families managing pediatric cancer treatments.
Can AI help reduce imaging frequency for children at low risk of pediatric cancer relapse?
Yes, AI has the potential to reduce imaging frequency for children identified as low risk of pediatric cancer relapse. By accurately predicting relapse risk based on previous brain scans, doctors may decide that less frequent monitoring is appropriate, thus minimizing the stress of frequent medical visits for these patients.
What role do longitudinal imaging techniques play in predicting glioma recurrence risk in pediatric patients?
Longitudinal imaging techniques are crucial in predicting glioma recurrence risk in pediatric patients as they allow AI models to analyze trends and changes over time. By evaluating a series of scans post-treatment, AI can detect early signs of cancer relapse that single images may miss, leading to timely interventions.
What research findings support the effectiveness of AI in pediatric cancer relapse prediction?
Recent research published in The New England Journal of Medicine AI demonstrated that an AI tool using temporal learning could predict glioma recurrence with an accuracy of 75-89%, significantly outperforming traditional methods that had about a 50% accuracy rate. These findings highlight the promising applications of AI in enhancing pediatric oncology outcomes.
How is the field of pediatric oncology evolving with the introduction of AI for cancer prediction?
The field of pediatric oncology is evolving significantly with the introduction of AI technologies for cancer prediction. These advancements enable clinicians to leverage sophisticated data analysis, improve early detection of relapse risks, and develop more effective, individualized treatment strategies, revolutionizing care for children facing cancer.
What challenges do researchers face in applying AI for pediatric cancer relapse prediction in clinical settings?
Researchers face several challenges in applying AI for pediatric cancer relapse prediction, including the need for further validation of AI models across diverse clinical settings. Ensuring the reliability and generalizability of AI predictions is essential before integrating these tools into routine pediatric oncology practices.
| Key Point | Description |
|---|---|
| AI Tool Development | An AI tool analyzes multiple brain scans over time to predict pediatric cancer relapse with greater accuracy than traditional methods. |
| Study Background | Conducted by researchers at Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, using data from nearly 4,000 MR scans across 715 pediatric patients. |
| Temporal Learning Technique | This novel method trains the AI model using a sequence of post-surgery MRI scans, enhancing its ability to predict recurrence. |
| Accuracy of Predictions | The AI model achieved 75-89% accuracy in predicting recurrence of gliomas, significantly outperforming traditional single image analysis (50% accuracy). |
| Potential Clinical Applications | Future clinical trials may utilize AI predictions to improve patient care and reduce unnecessary follow-up imaging for low-risk patients. |
Summary
Pediatric cancer relapse prediction is revolutionizing how we approach monitoring patients post-survival. The innovative AI tool introduced by researchers demonstrates that analyzing sequential brain scans not only enhances accuracy but can also tailor future patient care, minimizing the burden during recovery phases. As we continue to explore the implications of such technology, we edge closer to better outcomes for our children battling cancer.